What are fibroids? Causes, signs & treatments
Learn the signs of fibroids, the causes, and how to manage them
Fibroids are the most common gynaecological condition in the UK, with many of us developing them during our menstruating years. But what are fibroids exactly, and given they’re so common, should we be worried about them? Join Mooncup Advisor, Sophia, to get the low-down as she covers the need-to-knows about fibroids.
What are fibroids?
Uterine fibroids are non-cancerous growths that develop inside and around the uterus. Medically, people often refer to them as uterine myomas or leiomyomas, but these are a bit of a mouthful! The growths consist of muscle and fibrous tissue (hence the name fibroids) and can vary significantly in size. Some may be so small that they would be invisible to the naked eye, others can grow much larger to the size of a melon – and of course everything in between. Fibroids tend to grow slowly, most commonly appearing between the ages of 30-50, and may grow individually or in a cluster.
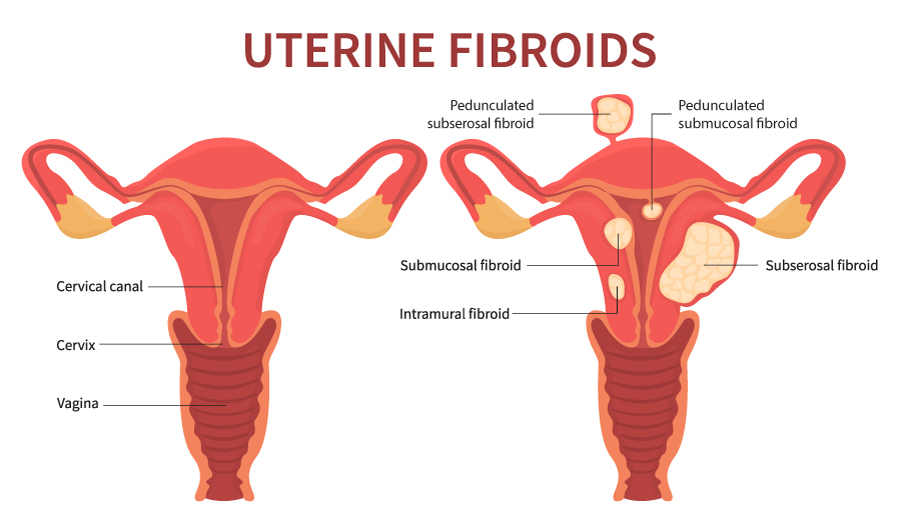
There are three main types of fibroid, each of which grow slightly differently:
Intramural fibroids grow within the thick muscle wall of the uterus. During a period, they can sometimes interfere with the blood vessels constricting effectively- and this can sometimes lead to heavier or painful periods. This is the most common type of fibroid.
Subserosal fibroids are closely connected to the outside wall of the uterus and can grow outwards into the pelvic cavity. Sometimes this can lead to them pressing on other pelvic organs such as the bladder, though they are often symptomless. Larger sized fibroids are more likely to be this type.
Submucosal fibroids grow closer to the inner wall of the uterus, underneath the endometrial lining (the layer that is shed during a period). If these get larger, they can grow into the space inside the uterus.
There can sometimes be a narrow ‘stalk’ of tissue that attaches the Subserosal or Submucosal fibroids to the uterus. When this is the case, they are called Pedunculated fibroids.
It’s possible to have different types of fibroids, of different sizes, all the at the same time.
What are the signs of fibroids?
So first up – often there are no signs of fibroids! Lots of us reading this now will have uterine fibroids but no idea about it. This is because quite simply, it’s not causing us any issues or symptoms! Although it’s very hard to estimate, and figures vary, it’s thought anywhere between a third and up to 80% of us with a uterus will develop uterine fibroids at some point in our life. However, because they are often symptomless, fibroids are frequently something that is incidentally picked up during different medical investigations. This can happen for instance during routine gynaecological examinations or during pregnancy ultrasound scans.
It’s thought that around a third of those with fibroids will however experience symptoms, and this seems to become more common after the age of around 30. Signs of fibroids include:
- Heavy, long-lasting or painful periods
- Bleeding between periods
- Tummy (abdominal) pain or pressure
- The abdomen feeling and appearing bloated
- Lower back pain or leg pain
- A frequent need to urinate
- Difficulties emptying your bladder
- Constipation
- Pain or discomfort during sex
- In rare cases, complications caused by fibroids can affect pregnancy and birth, or cause infertility
When to see your doctor
While many people with fibroids will have no symptoms, if you are experiencing any of the symptoms described above it’s important to make an appointment to see your doctor. They will be able investigate what may be going on. Your doctor is likely to take a history from you regarding any symptoms and the nature of your periods. They may also suggest a physical examination to see if they can feel anything that may indicate a fibroid. Because fibroids can be linked with heavy or prolonged periods, they may also recommend having a blood test to check for iron-deficiency anaemia.
Your doctor may then refer you for further investigations such as an ultrasound scan. From there, they can put in place a management or treatment plan.
What are the causes of fibroids?
This is still a bit of an unknown, and knowledge around the causes of fibroids is still developing. However, it’s thought that they are linked to the hormones oestrogen and progesterone. Fibroids tend to grow during the menstruating years when oestrogen and progesterone levels are at their highest. When levels of these hormones start to drop- for example when approaching the menopause- it’s common for fibroids to start decreasing in size.
There is also a link between early puberty and the development of fibroids. This may be due to having had higher levels of these hormones circulating in our body for a longer time.
Research also suggests that fibroids may have a genetic link and may run in families. This is particularly the case for those who have first-degree relatives with a history of them. Fibroids are also thought to develop more frequently in those of African-Caribbean origin.
Interestingly, childbearing history may also play a part. Those who have been pregnant are thought to have a lower risk of developing fibroids, with the risk decreasing further with the number of pregnancies.
Weight may also play a part on the incidence of fibroids in some cases, as being overweight leads to higher levels of oestrogen in the body.
Some studies have suggested that there may be a link between fibroids and Polycystic Ovarian Syndrome (PCOS). Some studies have also found links between fibroids and other health conditions, such as high blood pressure.
Can there be complications from fibroids?
Heavy or long periods due to fibroids can sometimes lead to anaemia or some vitamin deficiencies. If heavy periods is one of your symptoms, your doctor will be likely to suggest keeping an eye on your blood levels and may recommend iron supplements.
Depending on their location and size, fibroids can sometimes press on other pelvic organs such as the bladder or bowel. This can sometimes mean weeing or pooing becomes difficult, or that you need to go more often.
Although very rare, the stalk of pedunculated fibroids can sometimes become twisted. This can lead to severe pain and potential infection. Any severe pain should always be treated as a medical emergency.
While almost always benign (non-cancerous), extremely rarely a fibroid can be cancerous. However, it’s important to know that having fibroids does not increase the chance of developing a cancerous fibroid or any other types of cancer in the uterus. Your doctor should tell you more about this at your appointment.
Can fibroids affect pregnancy and birth?
While most of pregnancies and births won’t be affected by fibroids, sometimes it can create challenges. Again this will very much depend on the location, size and type of fibroid. Your midwife, doctor or obstetrician will be able to chat this further with you.
Sometimes fibroids may affect fertility. This can be by preventing the egg from implanting into the lining of the uterus, or sperm reaching the egg. Larger fibroids, particularly those that grow into the uterus, can also potentially block the fallopian tubes, preventing an egg from reaching the uterus.
In pregnancy, the increased levels of oestrogen can also sometimes cause fibroids to grow larger, though they often appear to shrink again after birth.
The most common fibroid-related symptoms during pregnancy are pain and bleeding – and you should always discuss these right away with your healthcare provider to rule out other potential causes. Large fibroids that grow into the space inside the uterus can reduce the space available for the baby to grow, or may affect the placenta. This can also increase the chances of pre-term birth and caesarean section. Sadly, it’s thought that some types of fibroids can increase the chance of miscarriage, but it’s important to remember this is rare.
How to manage fibroids
This is very much going to depend on what symptoms you have (if any), and the nature of the fibroids you have.
If your fibroids aren’t causing you any problems and were perhaps picked up incidentally during a different medical investigation, then your doctor may suggest ‘watchful waiting’. Essentially this means leaving things be, with periodic check-ups to monitor things. Over time your fibroids may eventually shrink, or even disappear – for example once you go through the menopause. That said, if you start to have symptoms, or feel these are changing in nature, it’s always important to share this with your doctor.
If your fibroids are affecting your life, then your doctor or gynaecologist may suggest various treatment options. The options will depend on the type and size of the fibroids you have, what impact they are having on you and your personal feeling about things.
Natural methods
Eating a healthy, balanced diet can help manage some of the symptoms related to fibroids. If you suffer from constipation, making sure you keep well hydrated and eating plenty of fruit, vegetables and high-fibre foods can all help alleviate this.
If you experience heavy or long periods, there’s a higher chance you may experience deficiencies of some vitamins and minerals including iron (anaemia). Upping your intake of iron-rich foods such as dark green leafy vegetables, pulses, iron-fortified cereals and drinks and dried fruits can all help. Your doctor may also prescribe iron tablets for you.
You can also check out lots of natural ways to help manage painful or heavy periods in these blogs:
Medication
Below you can find some treatment options your doctor is likely to suggest as a first step.
Hormonal medicines
Because of the hormonal link with fibroids, your doctor might suggest trying hormonal contraception to manage your fibroids. This could include the combined or progesterone only pill, progesterone contraceptive injection, or the IUS (hormonal coil).
Tranexamic acid
Doctors sometimes recommend this medication for those with heavy or prolonged periods. You take it during your period and it works by reducing bleeding from the small blood vessels in the lining of your uterus. It’s thought to be able to reduce blood loss by up to 50%.
Anti-inflammatory medicines
These can include non-steroidal anti-inflammatory drugs (NSAIDs), such as Ibuprofen and Mefenamic acid. As well as being painkillers, these medications can reduce the levels of prostaglandin being produced (a hormone linked to heavy periods).
Treatments that can help shrink your fibroids
If the treatments above are not helping or are unsuitable, then the following treatments may be suggested.
Gonadotropin releasing hormone analogues (GnRHas)
GnHHas can help shrink your fibroids. This medication reduces the amount of oestrogen produced, which can also stop you having periods. It can also relieve symptoms such as pressure on other organs such as the bladder or bowel. GnRHas are sometimes also used to shrink fibroids before you have surgery to remove them. Because it reduces oestrogen levels, this medication can produce some challenging menopause-like symptoms and is generally only prescribed for shorter periods of time.
Ulipristal acetate
This medication may be suggested, but it is less common. It works by blocking the effects of the hormone progesterone, which can then cause the fibroid to shrink. However, it’s not suitable for everyone and can have some side-effects, so your doctor will closely monitor you if you are taking this medication.
Non-surgical procedures
If your symptoms are severe and medication hasn’t helped, then a non-surgical procedure or surgery may be the right option for you. You’ll be referred to a specialist who can talk through potential options available to you depending on your individual situation. Non-surgical procedures include:
- Uterine artery embolisation (UAE) – this procedure involves blocking the blood vessels that supply the fibroids, causing them to shrink. It tends to be suggested to treat larger fibroids and is performed under a local anaesthetic by a radiologist.
- Endometrial ablation – this is a fairly minor operation that removes small fibroids within the lining of the uterus. You will usually be put under local or general anaesthetic and the procedure is generally quick to complete- around 20 minutes. The affected tissue will be removed using either laser energy, a heated wire loop, or hot fluid in a small balloon. You can often go home again the same day.
- MRI or Ultrasound guided procedures – these are fairly new, and so our knowledge around them is evolving. In these procedures MRI or ultrasound technology is used to locate and pinpoint your fibroids – these are then treated with heat, ultrasound or laser energy.
Surgery options
There are several surgery options available for treating fibroids:
Myomectomy
This type of surgery involves removing fibroids from the wall of the uterus. It’s performed under general anaesthetic and its suitability will depend on the type, number, size and location of the fibroids. The fibroids may be removed either though small incisions in your tummy (keyhole surgery) or a larger incision (open surgery).
Hysteroscopic resection of fibroids
This option may be suitable for smaller size fibroids growing or bulging into the uterus. Usually performed under general anaesthetic, thin instruments are inserted through the vagina and cervix and the fibroid tissue is removed the same way. A hysteroscopic resection doesn’t involve any incisions.
Hysteroscopic morcellation of fibroids
This is a newer procedure similar to the one above, but involves slightly different instruments. It may be suggested for those with a more complex history.
Hysterectomy
Hysterectomy is a surgical procedure to remove the womb. It’s the most effective way of ensuring fibroids do not grow back. Sometimes the surgery may also involve removing some of the attached organs such as the ovaries, fallopian tubes, cervix or lymph glands. Doctors would only generally recommend this if you have large, problematic fibroids, experience very heavy bleeding, and do not want to have children in the future. The surgery can involve a spinal, epidural or general anaesthetic. It can be carried out by keyhole or open surgery, or through the vagina. The NHS has further helpful information about hysterectomy here.
Remember that there is no one “best” treatment option when it comes to fibroids. Your symptoms, personal feelings, and thoughts about potential pregnancies in the future will all play a part in deciding what’s right for you. It’s important to talk through the benefits and potential issues relating to each option with your doctor – this will help you to make an informed choice on managing your fibroids.
Can the Mooncup help to manage fibroid symptoms?
The Mooncup can hold up to three times as much as a regular tampon, making it a great option for those with heavier periods!

The handy measurement markings on the side of the Mooncup® can also help you roughly measure your blood loss. This can be useful information to share with your doctor. As with any gynaecological condition, it’s always recommended to first check with your doctor that the Mooncup® is suitable for you to use.
Our friendly Advice Team, made up of medical health professionals, can send you a copy of the Mooncup usage guide to share with your doctor and are always happy to help with any questions. Feel free to get in touch with them at [email protected].
Did you enjoy this article? Head to this page’s footer to sign up to our mailing list to be the first to hear about our blogs!