Birth control options and advice – everything you need to know
Preventing pregnancy can be a confusing business, even though most of us will choose some form of birth control at some point in our lives. If you’re looking into contraceptive methods but unsure which one to choose, you’ve come to the right place. We’ll be exploring the various birth control options and what to consider.
Our guide to birth control options and choosing the right one for you
Controlling ones fertility is nothing short of complex, embroiled in politics, cultural beliefs, religion, relationship status and of course personal choice – though this is sadly not always first on that list. Let’s not forget that effective hormonal contraception has only been available in the UK on the NHS since 1961. It was restricted to married couples only until 1967.
The birth control options available for you will depend on where you live, but are also guided by personal suitability as well as choice. In the UK, you can find a wealth of information on contraception on family planning agency (FPA) and NHS websites. It is always best to discuss suitable contraceptive options for you with a specialist, such as your GP, local sexual health service or gynaecologist before you start a new method.
Before we take a tour of the most common birth control options, let’s brush up on a few basic menstrual cycle and sperm facts that can help us be in the driving seat, from the get-go!
- The average menstrual cycle is approximately 28 days long – but varies significantly from person to person. Day 1 is considered the first day that you start your period. The cycle lasts until the day before your next period begins. Regular cycles vary and can be shorter or longer than this. Anything between 21-40 days is considered within the normal range.
- Ovulation– when an egg is released from the ovaries and travels down the fallopian tube. This usually happens 10-16 days before your next period. A second egg might also be released, within 24 hours of the first egg. The egg is only viable for around 24 hours, so sperm must meet egg in that time frame for pregnancy to happen.
- Sperm can live up to 7 days in the female body. So if you have sex in the days leading up to ovulation, it is still possible to get pregnant. Sperm may well be first to the party – ready and waiting!
We all know that the word sex covers a multitude of varieties and may mean something different for all of us. However, for my purposes here, I’m referring to the vagina and penis kind of sex that may make you pregnant.
Ok, so get ready and strap in for the bumpy ride that is a whistle stop tour of 15 birth control options and what to consider.

Most common birth control options and what to consider
1. Natural family Planning
Natural family planning may be an attractive birth control option for Mooncup® users and for those who prefer a more organic approach. This method doesn’t intervene with the natural menstrual cycle or include taking hormones. It helps a lot if you have a regular menstrual cycle but still requires you to monitor a few signs very closely. Dedication and diligence are key here, though do not fear, your contraception specialist will help you chart this correctly and as accurately as possible.
Natural Family Planning as a birth control option – what to consider
- Knowing the length of your menstrual cycle is very important for calculating your most fertile days! Watch out though, as your cycle can vary from one month to another. It can also be affected by illness or medications, stress, time zones and travel. It is often advised to track your cycle over a year to better understand your average cycle length. As you may have already discovered, there are many period tracking apps out there that can help with this.
- Daily temperature readings. Our body temperature rises ever so slightly after ovulation. Temperature readings need to be done using a digital thermometer or one specifically used in natural family planning due to the precision needed. First thing in the morning is usually advised and before eating, drinking or smoking.
- Checking your cervical mucus. – You can do this by inserting a finger into your vagina up to approximately your middle knuckle. The mucus can be tricky to analyse with confidence, but vaginal discharge does change throughout the menstrual cycle and hopefully you will soon become a pro at spotting the difference throughout your cycle. Importantly, on the most fertile days, the mucus can feel wetter than usual and have a similar texture to egg white.
- Being tuned into to your cycle gives you a clearer picture of your fertile window. It can of course also help you to conceive as well as to avoid it.
- Remember- using barrier methods such as a condom or Diaphragm together with natural family planning in the most fertile days is essential. The other option is to not have sex during this time.

Barrier methods
These birth control options pretty much speak for themselves, acting as a barrier and preventing sperm meeting an egg. Again, if used correctly they can be very effective. However, as always, there are a few things to bear in mind.
2 – Male condoms
Condoms are made from thin latex (rubber) and available in a myriad of textures, colours, flavours and sizes. They should be worn over an erect penis only, as otherwise the condom will slip off and become ineffective. Oil-based products, such as creams, lotions and moisturisers, including petroleum jelly (or ‘Vaseline’), should not be used with condoms as they can damage the material and render the condom unsafe to use. Water-based lubricants are safe to use. Latex allergy or sensitivity is also a consideration, although Latex-free condoms are widely available.
It is important to first check the expiry date for each condom. In the UK, condoms that are tested to the highest quality will have a BSI kite mark on the packet. Be careful with long nails as condoms can tear easily, and if they do you may need to consider emergency contraception (more about this later). The great thing about condoms is that they can also protect you against Sexually Transmitted Infections (STI’s), though I’m sure you already knew that!
3 – The Female condom
The female condoms are also made from either latex (rubber) or synthetic latex. Similarly, expiry dates and manufacturing marks should be checked on each pack before use. The female condom is placed inside the vagina before sex using the smaller of the two rings. The larger ring sits around the opening of the vagina. It may seem obvious, but the penis must go inside the condom and not to one side (between the condom and vaginal walls). Female condoms are strong, but if you notice any tears or breaks to the material after use, you may need to think about emergency contraception. Also helping to protect against STIs this can be a good choice for many.
C-Card scheme is available for all young people ages 13 – 24 in the UK, and it is funded by the NHS. Once registered (usually in your local sexual health service), young people can access free condoms, lube and dams (usually latex sheets used for oral/vaginal/anal sex to help protect against STIs). Many organisations, such as sexual health clinics, some GP surgeries, pharmacies and other youth agencies, are part of the C- Card scheme.
4 – The Cap & Diaphragm
A contraceptive diaphragm or cap is a round dome made of thin, soft silicone or latex. It is used with a spermicide gel (to stop sperm in their tracks) and inserted into the vagina before sex. It covers the cervix (neck of womb) so sperm cannot get into the womb to fertilise an egg.
Cap & Diaphragm – what to consider
- Can be very effective at preventing pregnancy if used as instructed along with spermicide gel.
- Like the Mooncup menstrual cup, the diaphragm or cap is a new skill to learn and can take a few goes to get right. Your doctor, nurse or gynaecologist will explain how to use it. But don’t worry as it can soon become second nature.
- Diaphragms and caps come in different sizes. You will need to be measured by a professional to make sure you have the right fit for you.
- The diaphragm or cap needs to be kept in place for at least 6 hours after sex.
- If you experience cystitis type symptoms, you will need to speak to your doctor and may need to switch to a smaller size.
- If your weight changes, or if you have a baby you may also need to review the size.
- Be aware of latex allergy. It might also be helpful to know that spermicide gel can cause irritation for you or your sexual partner/s.
- It is not advised to use a cap or diaphragm during your period due to a possible link with Toxic Shock Syndrome (TSS). Although rare, this can be a life-threatening condition. While we are here, you may also wish to see what we say about Mooncup® use and TSS.
- A bit like your Mooncup – it does need to be cared for according to the instructions that come with it. Keep an eye for any signs of damage such as rips or tears, and look up how best to clean it. Please note that cleaning recommendations are very different to those of the Mooncup menstrual cup

Hormonal birth control options
In a nutshell, many of today’s birth control options contain synthetic (man-made) hormones that work similarly to our natural hormones – progesterone and oestrogen. Certain hormonal birth control options may not be right for you depending your age, weight, whether you are a smoker, your medical history or if you are taking any other medicines. Your health care practitioner will be best placed to assess and discuss the best options for you.
Progesterone & oestrogen birth control options
5 – The combined pill
Often just referred to as “the pill”, it contains forms of both progesterone and oestrogen. It is extremely effective at preventing pregnancy when taken as advised, but can become less effective if you miss a pill, take it alongside certain other medications, vomit or have bad diarrhoea.
The combined pill – what to consider
- The pill prevents ovulation, but also thickens the mucus in the neck of the womb, making it difficult for sperm to enter the womb and reach an egg.
- The lining of the womb becomes thinner so there is less chance of a fertilised egg implanting into the womb and being able to develop.
- There are different procedures for taking the combined pill depending on the type of pill you take, so be sure to discuss this with a medical health professional.
The combined pill – potential side effects
Potential side effected for the combined pill include headaches, nausea, breast tenderness, changes to mood. Side effects usually settle after the first few months of taking the pill but if they continue, do talk to your doctor, gynaecologist or nurse. They may occasionally need to adjust the level of either hormone by changing the type of pill. There is also a very low risk of more serious side effects, such as blood clots and cervical cancer. On the plus side, the combined pill may help if you experience heavy periods or painful periods, PMS or Endometriosis, but again you should always discuss your concerns with your doctor, nurse or gynaecologist. There is no current evidence that the pill will make you gain weight.

6 – The Patch
The patch contains both progesterone and oestrogen and prevents pregnancy in the same way the pill does. This sticky patch can be put on many places on the body, except your breasts or on sore or hairy skin. It’s good to mix it up a bit in terms of where you stick it, too! Unlike the pill it slowly releases the hormones through the skin and into the bloodstream.
The patch as a birth control option – what to consider
- The patch needs to be changed weekly, then stopped for a week, in which time you should have a bleed – similar to a normal period.
- Because the hormones are absorbed through the skin it remains effective if you vomit or have diarrhoea.
- If you have heavy or painful periods, the patch can help.
- You can bathe, swim and do your normal exercise routine while wearing the patch.
- Temporary side effects can include headaches, breast tenderness and nausea. In very rare cases people using the patch may develop a blood clot in a vein or an artery.
- The patch may protect against womb, ovarian and bowel cancer.
- The patch is very sticky, but if it does fall off – be sure you know what to do!
- Research suggests that people who use the contraceptive patch have a small increased risk of being diagnosed with breast cancer compared with those who don’t. This reduces with time after stopping the patch.
- Research also suggests there’s a small increase in the risk of developing cervical cancer with long-term use of oestrogen and progestogen hormonal contraception.
7– Vaginal ring
The vaginal ring, aka NuvaRing, is a small, soft, plastic ring that you insert inside your vagina. It releases a continuous dose of oestrogen and progestogen into your bloodstream. The ring prevents pregnancy in the same way as the patch and pill, by stopping ovulation and thickening the cervical mucus.
Vaginal ring – what to consider
- It is highly effective at preventing pregnancy when used correctly.
- You change the ring every 3 weeks so don’t have to think about it every day.
- You can have sex while wearing the ring.
- Unlike the pill, and similar to the patch, the ring still works if you vomit or have diarrhoea.
- The ring may help with PMS, and your bleeding can be lighter and less painful.
- Possible temporary side effects can be similar to the pill and patch, though can also include an increase in vaginal discharge.
- The risk of developing a blood clot when using the ring is low.
- If the ring comes out of the vagina, it needs to be rinsed with water before re inserting it as soon as possible. Contact your health care professional for advice if you think it’s been a while since it came out!

Progesterone-only birth control options
8 – The progestogen-only pill
The progestogen-only pill is sometimes also known as the ‘Mini Pill’ or the POP. Just to confuse us, there are now two types. The 3-hour progestogen-only pill – is the traditional progestogen-only pill and must be taken within 3 hours of the same time each day. The 12-hour progestogen-only pill (desogestrel progestogen only pill) must be taken within 12 hours of the same time each day. It prevents pregnancy by thickening the mucus in the cervix to stop sperm from reaching an egg. The 12-hour POP can also stop ovulation.
Progesterone-only pill – what to consider
- To work effectively, the progestogen-only pill needs to be taken every day with no breaks between packs.
- You must be on time with taking the pills. Remember there are two different types, make sure you know which one you have!
- If you’re vomiting or have bad diarrhoea, the progestogen-only pill may not work.
- Your periods could change completely. They could become lighter, less frequent or stop completely.
- Side effects can include spotty skin, breast tenderness, nausea or vomiting, headaches including migraines, mood changes or changes to libido. Most side effects usually go after a few months of taking the POP, if not, talk to your doctor. Some people can also develop small fluid-filled sacs (cysts) on their ovaries. These are usually harmless and disappear without treatment.
- The POP can be a good alternative if you cannot take methods that include oestrogen.
- There is continued research into the link between breast cancer and the progestogen-only pill. There is currently not enough evidence to say that the POP does not increase the risk of breast cancer. If there is any increased risk, it’s likely to be very small and will disappear with time after you stop taking the progestogen-only pill.
9 – Contraceptive injection
Contraceptive injection is another progesterone-only method. The injection releases progestogen into your bloodstream to prevent pregnancy.
The injection works by preventing ovulation. It thickens cervical mucus and thins the lining of the womb so a fertilised egg is less likely to implant itself. The injection lasts for 8-13 weeks – depending on the brand. You may be offered a special version of the injection that you can give to yourself. This can be given in your thigh or tummy. If given by a clinician you will likely be given the injection in your bottom.
Contraceptive injection – what to consider
Some of the advantages:
- Unlike some of the other methods, it’s not affected by other medicines.
- It may reduce heavy or painful periods and help with PMS.
- Your contraception is covered for 8-12 weeks at a time, depending on the type of injection.
- You can use it while breastfeeding.
Some disadvantages:
- Your periods may change and become irregular, heavier, shorter, lighter or stop altogether. This can carry on for some months after you stop the injections.
- Potential side effects include headaches, acne, decreased sex drive, mood swings and hair loss. These can continue as long as the injection lasts (8 or 13 weeks) and for some time after.
- It can take up to one year before your periods return to normal though you can become pregnant in that time.
- Some people can put on weight when they use contraceptive injections. Though this may be an advantage for some.
- As with all injections- there’s a small risk of infection.
- The injection affects natural oestrogen levels, and it can affect your bones. Your clinician may recommend you stop using this method after two years of use to prevent any long-term affect.
- Rare allergic reaction.
10. – Contraceptive implant, aka ‘the implant’
The implant is a small plastic rod that’s placed under the skin of your upper arm by a doctor or nurse. It releases progestogen into your bloodstream, prevents ovulation and thickens the cervical mucus as well as thinning the lining of the womb to prevent pregnancy.

Contraceptive implant – what to consider
- The implant is very effective and you’re good to go for the next three years. It can be a good option if you are likely to forget taking or changing something on a regular basis.
- The implant requires a minor procedure for its insertion and removal. This must be carried out by a doctor or nurse. If the insertion site becomes infected you will need to see your doctor.
- Once removed, your natural fertility will return very quickly.
- You may feel some bruising, or swelling around the implant when first inserted. If the shape of the implant changes or you cannot feel it, you will need to talk to your fitter.
- Your periods can become irregular, lighter, heavier or longer.
- It is common for your period to stop completely or become irregular. Although not harmful, you may prefer to have periods!
- You can have the implant fitted any time after you’ve given birth. It is considered safe to use when breastfeeding your baby.
- You may experience temporary side effects like nausea, breast tenderness, headaches or mood swings during the first few months.
- Your acne might get worse or you may develop spotty skin.
Intrauterine birth control options
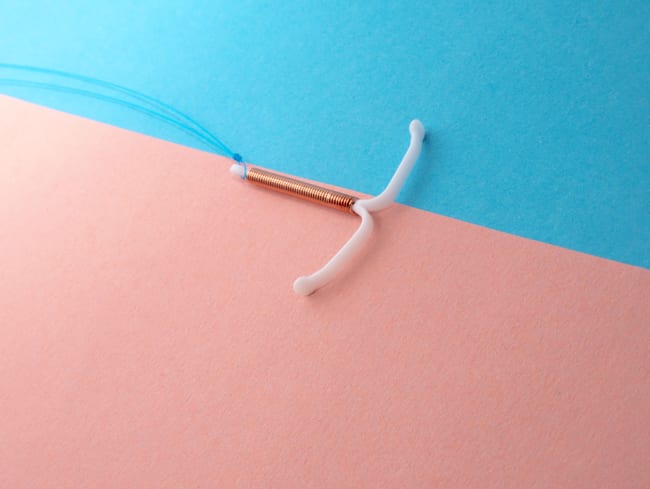
11- The IUD
Often referred to as ‘the coil,’ the IUD is hormone-free and usually a small plastic & copper device which is placed into the uterus (womb) by a doctor or nurse. It lasts for 5-10 years, depending on the type, and protects you against pregnancy by releasing copper into the womb. The copper changes the cervical mucus making it more difficult for sperm to reach the egg. It may also stop a fertilised egg from implanting in the womb.
The Mooncup and Intrauterine contraception ie. IUD or IUS
We know that there are Mooncup® users who are happily using their menstrual cup alongside an IUD/IUS (coil). However, there have been some instances where an IUD/IUS has become dislodged when using the two together. We recommend talking to your IUD fitter before using the two devices together. For more information please have a peak at our IUD FAQ.
IUD – what to consider
Positive points
- Extremely effective at preventing pregnancy when correctly positioned.
- There are no hormonal side effects like breast tenderness, acne or headaches.
- It’s not affected by other medicines.
- Once the IUD has been removed, your fertility returns very quickly.
- If you’re 40 or over when you have an IUD fitted, it can be left in until you reach the menopause or you no longer need contraception.
- An IUD can usually be fitted four weeks after giving birth (vaginal or caesarean). In some cases, it can be fitted within 48 hours of giving birth. It’s also safe to use when you’re breastfeeding.
Not so positive points
- Your periods can be heavier, longer or more painful in the first few months after your IUD is fitted.
- If periods are heavier due to the IUD, your Mooncup might come in handy. Because the Mooncup has some nifty measurement markings, you can keep an eye on the amount of blood you lose.
- You may get spotting or bleeding between periods.
- There’s a small risk of getting an infection after fitting.
- There’s a small risk that your body pushes the IUD out, or it can move out of place. Your doctor or nurse will teach you how to check the threads to know it’s in place. If you are unsure always check with your fitter.
- The insertion procedure can be uncomfortable.
- Signs of infection can include: fever, tummy pain, abnormal or smelly vaginal discharge. In this situation, you know what to do!
- If your partner can feel your threads during sex and it is uncomfortable, see your fitter for further advice.
- If the IUD fails and you become pregnant, there’s an increased risk of an ectopic pregnancy (a fertilised egg that implants itself outside of the womb). This can be very serious and needs urgent medical attention.
- In rare cases, when the IUD is inserted, it may slightly puncture the womb. This can be painful, although sometimes there may be no symptoms.
- There is some research to suggest that you may have a higher chance of having recurrent thrush.
12 – The IUS
Sometimes referred to as the ‘hormone coil’, the IUS is a small, T-shaped plastic device that’s inserted into your womb (uterus). Unlike the copper IUD, it releases progestogen to stop you getting pregnant. The coil lasts for three to five years, depending on the type. It works by thickening the cervical mucus, which makes it more difficult for sperm to get through the cervix, and thining the lining of the womb so an egg is less likely to implant itself. For some, it can also prevent ovulation, but most people continue to ovulate. The advantages and disadvantages are similar to those of the IUD. The main difference is that you may experience some hormonal side-effects such as:
- mood swings, headaches, acne or breast tenderness
- An uncommon side effect of the IUS is small fluid-filled cysts on the ovaries. These usually disappear without treatment.
13 – Emergency contraception
Emergency contraception can be used to prevent pregnancy if the contraception you have used has failed or after unprotected sex, a condom you used may have split or come off, you may have missed taking the pill, or forgotten to renew your patch or vaginal ring.
There are two types of emergency contraception:
- The emergency contraceptive pill, sometime known as the ‘morning after pill’ and
- The intrauterine device (IUD or coil).
Your healthcare professional will be able to explain the best options for you. Emergency contraception is free of charge from your local sexual health service clinic, but you can also buy it from most pharmacies, in person or online. You may need to run through some questions first. The cost varies but is usually in the region of £25 – £35.

And now for something completely different.
Sterilisation as a more permanent birth control option
Male and female sterilisation are both more permanent procedures, rather than methods of contraception. In many cases this choice will warrant significant consideration and discussion.
14 – Vasectomy
A vasectomy requires a surgical procedure, which is usually carried out under local anaesthetic, though can also be done under general in rare instances. The procedure doesn’t usually take very long and is very effective at preventing pregnancy. It works by cutting or blocking the small tubes (vas deferens) that transport sperm from scrotum to the penis.
Vasectomy – what to consider
- You can expect to be invited for some form of counselling (more of a discussion) before the procedure.
- The procedure usually takes around 20 minutes.
- As with any surgery, there’s a small risk of infection.
- It is not an easy procedure to reverse.
- It should not affect the male libido or ability to enjoy sex. They will still have erections and ejaculate, but the semen won’t contain sperm.
- It takes a while for the operation to become effective and so an alternative form of birth control should be used in the interim. This is usually around three months or so.
- It is usually advised not to have sex for at least one week.
- It is important to discuss aftercare and what to expect after the procedure.
- Around three months after the procedure, a semen sample will be collected to check for sperm. Until this time, there may still be a risk of pregnancy.
15– Female sterilisation
Female sterilisation works by blocking the fallopian tubes (the tubes that carry the egg from the ovaries to the womb). It works usually either by applying clips or rings, or by tying, cutting and removing a small piece of the tube. The surgeon or gynaecologist should discuss the operation in full with you beforehand.
Female sterilisation – what to consider
- Extremely effective at preventing pregnancy.
- Periods will continue and there is no impact to hormone levels.
- Another form of contraception will be needed for a while after the operation.
- As with any surgery, there’s a small risk of complications.
- If the operation is unsuccessful, there may be a risk of ectopic pregnancy.
- Sterilisation is very difficult to reverse, so it is not a decision to be taken lightly.
And so there we have it, a brief look at the most common birth control options. It may be a lot to digest and think about, but there is an abundance of support and information out there for grabs. This was merely a snippet. Above all – remember you have choices, so discuss them!
The Mooncup® and birth control options
You may have questions about using your Mooncup® alongside some of the contraceptive methods. It might help to know that the Mooncup is designed to be used for the length of an average menstrual bleed; around 5-7 days. If your period goes on for longer than usual, or happens more frequently than the average period bleed (for example this can happen when taking hormonal contraceptives), do not hesitate to get in touch with our friendly advice service, run by medical health professionals here at Mooncup Ltd. From there we can further discuss how to best use your Mooncup.
The Mooncup® is a great way to be more in tune with your cycle. Find out more and get yours here.
You might also be interested in:
More orgasms please!
How to choose the best menstrual cup for you?
How to hack your cycle and own your period superpower
What are the different types of vaginal discharge and what do they mean?
The colour of your period: what does it mean?
Period tracker apps: when technology met menstruation